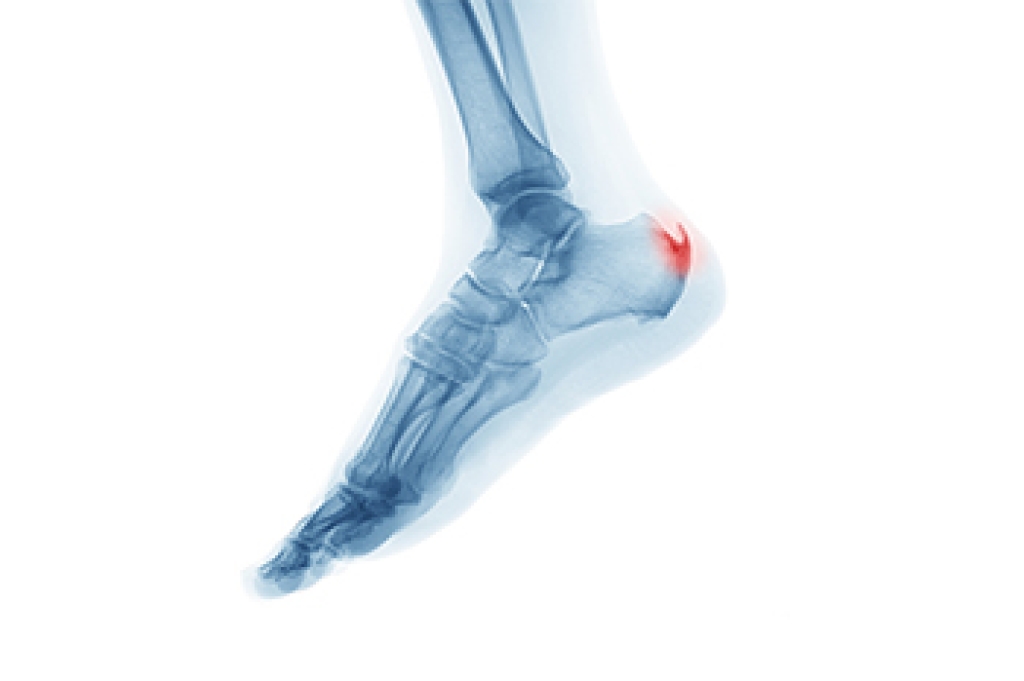
A heel spur is a bony growth that develops on the underside of the heel bone, often where the plantar fascia attaches. It typically forms over time as a response to ongoing stress or pressure on the foot. One of the main contributing factors is aging, as the tissues naturally lose elasticity and strength. Abnormal stress from repetitive activities, poor foot function, or walking patterns can place excessive strain on the heel. Carrying extra weight increases the load on the feet, which can lead to small tears in the plantar fascia. These micro-tears trigger inflammation and can encourage calcium deposits to build up, forming a spur. If you have heel pain, it is suggested that you schedule an appointment with a podiatrist who can accurately diagnose and treat heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Cary Golub, DPM from New York. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions, please feel free to contact our offices located in Williston Park, and Long Beach, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.




